Sample report for the Prolaris genetic test .
First, let's clear the air.
Why do I blog about my prostate cancer and the assorted tests, treatments? Well, let's start with the fact this is the second leading cancer killer of men, up to 30,000 a year. But that often takes no account at all of the hell many men endure in terms of the tests (like biopsies) as well as treatments - often described as more savage than the disease. One can scan and google but unless one is actually a member of a prostate cancer survivor group (as I am) he or she will have scant idea of the pain and suffering aroused by this disease, including in spouses.
Thus, the point here is not anything to do with some narcissistic disease obsession but rather getting information out about how one might very well have to deal with this cancer - especially after recurrence. (More men than you think, in fact, kill themselves after undergoing treatment then having the cancer recur - on being plunged into deep depression).
The other aspect is to show not all cancer narratives are of the saccharine form, e.g.: 'I beat the cancer and it never came back! NO, that's a tall tale, one often peddled by a sappy PR-based media and lackeys that don't know any better, or have an agenda to avoid any negativity. But, they avoid mentioning that in nearly 1 of 3 instances prostate cancer returns, even for those who have radical prostatectomy.
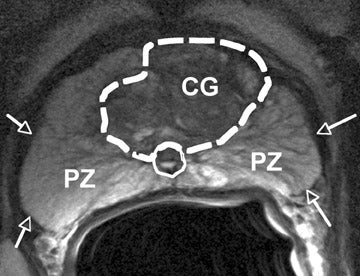
Six days ago, the local urologist's office phoned to tell me the result of the Prolaris genetic test (of tissue extracted at my MRI fusion biopsy) was that the prostate adenocarcinoma was aggressive. To fix ideas, the sample shown on the image above yields a score of 3.0 and is in the "less aggressive" region. This in concert with other clinical-pathologic values enabled an estimate for a 10-year prostate cancer-specific mortality risk. This patient then has a 10-year prostate cancer specific mortality risk of 2%..
My score by comparison was 6.6, corresponding with a 12.5 % specific risk of mortality at ten years. That translates to a 1 in 8 probability of croaking from it if I decided to do nothing. While this sounds like a fair risk to take for many, it would be roughly analogous to walking through a South Side Chicago neighborhood at 3 a.m. and expecting to get back home in one piece. In other words, a no go. In addition, it leaves out all the nasty side effects you'd have to deal with if the cancer breaks out of the capsule (metastasis) which it is now on the verge of doing given the "perineural invasion" cited in my recent post on the MRI fusion biopsy result, e.g.
http://brane-space.blogspot.com/2016/09/biopsy-result-shows-writing-on-wall.html
It is via the nerve pathways by which the cancer escapes, gets into the bones (bone mets) as well as lungs, etc. The PET scan image below shows bone mets even in the spine. Each met is in reality a locus of prostate cancer.

The question for the medical assistant who phoned was: What is the risk of metastasis? She gave me the five year risk of metastasis as 39.5% or nearly 2 in 5. Again, if I chose to do nothing.
Since then, with further research, including gleaning insights from a prostate cancer survivors' group called Team Inspire, I have opted to do a salvage treatment known as focal cryotherapy. This will entail a 150 point 3D staged biopsy. Then that will be used as a guide to freeze the specific tumor regions in the gland. It is described as an "outpatient treatment" but done under general anesthesia, see e.g.
https://www.youtube.com/watch?v=-OnqA-mJDWg
The plan is to have it done at the University of Colorado Anschutz Center, with focal cryotherapy specialist Dr. E. David Crawford, e.g.
http://www.edavidcrawford.com/targeted-prostate-cancer-treatment
A phone consult with Dr. Crawford's medical assistant, after seeing the MRI fusion biopsy and Prolaris reports, indicated I had the leeway to wait into until the new year to get it done. This meant not having to contend with any side effects, etc. during the holidays. In addition, Janice six days ago experienced a mini-stroke (TIA or transient ischemic attack) so that means she must also get much better before we can move forward . I suspect all the tension with Trump and this election played no small role in her attack.
Anyway, I will need to have a preliminary meeting with Dr. Crawford in November, at the Aurora UC center, then we will discuss when to have the biopsy and the treatment. The latter, I am informed, is usually done at least two months later to allow enough healing time after 150 sticks through the perineum.
By now most everyone has also seen or read of actor Ben Stiller's bout with prostate cancer, e.g.
http://www.cnn.com/2016/10/04/health/ben-stiller-prostate-cancer/
But what they may have ignored is how the treatments and testing can often be worse than anything else - especially if one has a slow growing cancer. The risks of further tests, treatments include sexual impotence and incontinence The latter means wearing diapers - as in Depends - permanently. This is also why Otis Brawley of the American Cancer Society, has warned that most men need to be very careful before stepping through that testing and treatment door. Nine times out of ten the cancer will be so slowly growing that you can do 'watchful waiting' - especially for Gleason scores of 6 or less.
Once you go further - based on the PSA test- be prepared for the biopsy which doesn't always treat a lot of men very well, not only the pain but possible sepsis, or other complications (e.g. incontinence). And if you decide to act on the biopsy results, be prepared for having to decide which treatment is best for you, realizing whichever you choose is a crap shot. As one member of Team Inspire put it (perhaps a tad hyberbolically):: "If there's even one cancer cell left it can grow back."
Well, if there is tissue left at the margins after a surgery, it certainly can!
See also:
https://www.youtube.com/watch?v=HDGAQdHid1c
And:
http://brane-space.blogspot.com/2012/09/thge-longest-dayand-then-some.html
And:
http://brane-space.blogspot.com/2012/10/is-there-sex-after-prostate-cancer.html
And:
http://brane-space.blogspot.com/2012/10/penile-rehabilitiation-what-most-docs.html