Robert Nagourney ('Every Cancer Patient Is One In A Billion', WSJ, July 22, p. A15) is correct when he writes:
"We now know that cancer is a disease of altered cell survival, not excessive proliferation. That is, cancer doesn’t grow too much, it dies too little. Applying cell kinetics, we can trace a newly diagnosed colon cancer back to its first cell. This reveals that a cancer that has spread to the liver by the time it’s diagnosed may have its origins some 30 years earlier yet remain undetectable with current diagnostic techniques for well over two decades. The same holds true for pancreatic, lung and other tumors. By the time many patients are diagnosed, they have unknowingly lived more of their lives with cancer than without. "
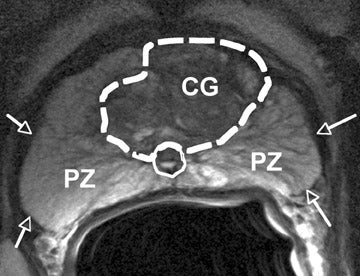
Which knocks out the trope that cancer is an "uncontrolled over growth" of cells. In reality, it is cells not 'clocking' out and dying on schedule. Let's go to the image shown at the top. This highlights what happens to a cell when a specific protein (p27) messes up its death- cessation time. To be specific, in one particular shape the protein prevents cell division, in another it won't. In the latter case there is the potential for what we call cancer - the cell ceasing to terminate.
Given a cancer can take decades to be detected it begs the question that if this is the case then why not just allow for continued co-existence? Say as opposed to carving it out - leaving much damage in the wake, or burning it out (by radiation), or freezing it out, e.g. by insertion of cryotherapy probes at -90F ,

Why not just live with it and done? Well, because to most cancer patients it represents an 'invader' and foreign invaders are not to be tolerated. So one carves, burns or freezes them out. But if they've already been there for years, maybe decades, then why not let them remain longer- so long as these cells don't pose mortal threats - say invading critical organs?
Hell, advanced prostate ("metastatic") cancer patients already do this once the cancer has resisted all standard treatment approaches and therapies - as indicated above. They snatch extra years by resorting to hormone treatments such as androgen deprivation therapy (ADT) generally suppressing testosterone - the key "food" for prostate cancer cells, see e.g. .
https://www.youtube.com/watch?v=KtIfsvQh2qI
This is despite there being a faction of cells known as "hormone treatment insensitive" that keep on growing. As pointed out by Hopkins urologist Patrick Walsh in his book Dr. Patrick Walsh’s Guide To Surviving Prostate Cancer’. p. 338):
"Hormonal therapy does two things: it stops cells from making PSA, and it shrinks the hormone sensitive cell population. Thus, a man's PSA falls and it takes longer for his bone scan to become positive for metastases. But it doesn't stop the clock. The hormone insensitive cells keep right on growing silently."
But the main issue for the advanced patient is to prevent the "mets" as seen in the PET scan below, from wreaking havoc by spreading to major organs:

From getting out of control, causing bone fractures and the like or getting into critical organs like the liver.
Nagourney's other point is equally important (ibid.):
"Cancer cells are normal cells that distort physiologic stress responses to succeed under conditions of deprivation. Drawing on genetic elements, either mutated or normal, they configure a new biology: the cancer phenotype. Since there are some 1,000 cancer-related genes and each cancer requires up to three distinct gene alterations to succeed, every cancer patient is literally one in a billion. It’s reminiscent of Tolstoy’s observation: “All happy families resemble one another, each unhappy family is unhappy in its own way.”
Note the numbers: 1,000 cancer-related genes, and up to three distinct gene alterations to succeed. Do the combinatorial math and every cancer patient is like a 1 in a billion manifestation. This belies the "manfiest complexity" of the disease as Nagourney puts it but also indicates the "one size fits all" treatment response to most cancers (e.g. surgery, chemo, radiation) is passe. This is given the one size fits all template is based on the error of applying population statistic to an individual for whom the gene(s) involved and alternations call for something totally different. As the author describes the situation:
"The physician’s role is to discern what makes each patient unique, but few take the time to find out. While gene profiling offers hope, cancer has proved much more complex than the sum of its genes. The study of human tumors at the tissue level suggests that it may be possible to reverse-engineer the process by moving away from top-down genomic analyses toward bottom-up cellular studies. The Physical Sciences Oncology Network is applying physical principles to cancer medicine to explore the dynamics of human tumors in three dimensions. One concept is that in select patients less may be more, since responses can be prolonged using intermittent dosing.
Cancer-cell defenses can now be examined in the laboratory by using drugs, gene-targeted agents and inhibitors of cellular metabolism to probe human tumor biology. We can ask: What cell survival process is your cancer using? More important: Can it be targeted therapeutically? If the answer is yes, and a drug or combination is identified, the patient would likely respond favorably—twice as likely in fact. But if the answer is no, treatments would be more likely to cause suffering without benefit."
Which is sad. The last is especially germane whether we're talking about a patient like my brother Mike (who died in June last year) offered chemo and radiation to get "a few months" more from stage 4 liver cancer, or a prostate cancer patient having to make the choice to get hormone therapy to extend life - even at the risk of getting Alzheimer's disease. These considerations have been raised in a forthcoming book ('The First Cell, and the Human Costs of Pursuing Cancer to the Last') by Dr. Azra Raza
Most telling is the author's response to one cancer patient for whom a 2-drug chemo combination had provided a remission that's lasted ten years. When the patient asked him "You mean I'm not going to die?" He responded: “No, you’re not sick. You just have cancer.”
In other words, having cancer and dying from it may actually be two mutually exclusive propositions. The trick is to decide or determine which one applies in the case of a particular individual. For my own part I have decided for the time being to live with the existing cancer given I am asymptomatic. At such time that changes, say manifesting in bladder obstruction or bone pain, then it will be time to go the ADT route. But I am hoping that can be postponed as long as possible!
See also:
Cancer Treatment at the End of Life-
https://www.nytimes.com/2019/08/05/well/live/cancer-treatment-at-the-end-of-life.html
Excerpt:
Excerpt:
"Although slightly more than two-thirds of cancer patients treated in the United States are cured, this is mostly the result of early detection and combinations of surgery, radiation and chemotherapy treatments developed decades ago, Dr. Azra Raza, director of the Myelodysplastic Syndrome Center at Columbia University, wrote in her forthcoming book “The First Cell, and the Human Costs of Pursuing Cancer to the Last.” In fact, experts suspect that some cancers discovered through early detection would never have become fatal even if they had not been treated.....As Dr. Raza wrote, most new cancer drugs add mere months to a patient’s life at an agonizing physical and financial cost
The decision today is more complicated that in decades past because some modern treatments are less toxic than traditional chemotherapy and because there are now ways to counter, though not necessarily eliminate, the devastating side effects of many treatments."
And:\
Latest Medical Finding: Hormone Treatments Put Pr...